Module 1: Knowledge of Technology
- Description
- Curriculum

-
1Contents
Course description
What will i learn?
- Knowledge: · Understand the principles and importance of remote patient monitoring · To learn how use remote patient monitoring with telehealth · To help patients use at-home health monitors
- Skills: To develop basic skills in assisting people in need remotely over telehealth systems.
- Competence: The acquisition of the necessary knowledge for applying telemetry at the Point-of-Care and collaborating remotely.
Requirements
- English Language
-
2Module 1: Knowledge of Technology
Module 1: Knowledge of Technology
Introduction
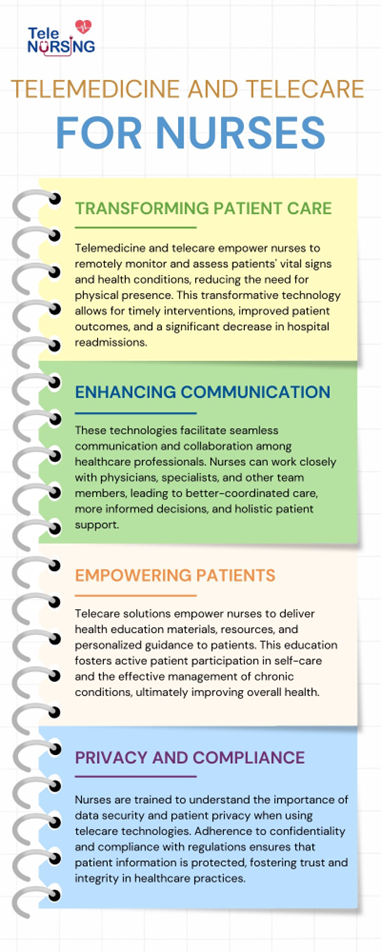
Telemedicine can play a crucial role in monitoring and managing chronic conditions. Nurses can remotely monitor patients with chronic illnesses, adjust treatment plans as needed, and intervene promptly if any health issues arise. Telemedicine platforms facilitate communication and collaboration between nurses, physicians, and other healthcare professionals. This seamless communication can lead to better-coordinated care and improved patient outcomes. Through these technologies nurses reduce the need for to travel to patients' homes or for patients to visit healthcare facilities unnecessarily. This not only saves time for nurses but also helps optimize healthcare resources and reduces costs for both patients and healthcare providers.
Telecare solutions can help nurses and care providers stay connected with their patients, even during periods when in-person visits may not be possible or advisable. This continuity of care can foster stronger patient-nurse relationships and improve patient engagement. Telecare platforms can deliver health education materials and resources to patients, empowering them to manage their conditions effectively. Nurses can remotely provide guidance and support to patients in self-care and disease management.
Overall, telemedicine and telecare technologies offer valuable tools for nurses and care providers to provide high-quality care, improve patient outcomes, and increase healthcare accessibility for diverse populations. It is essential for nurses and other healthcare professionals to be well-trained in utilizing these technologies to maximize their benefits in supporting patient care.
-
3LESSON 1 Remote Patient monitoring
Introduction
Remote patient monitoring (RPM) is a telehealth innovation that offers significant opportunities to increase the timeliness of care, enhance health outcomes, and potentially reduce hospitalisations and associated healthcare costs.[1] RPM uses technology to observe a patient’s physiological (eg, heart rate, blood pressure) and behavioural (eg, medication adherence, physical activity) information from a distance.[2] With support, many individuals could effectively self-manage chronic conditions in the community.
Remote patient monitoring (RPM) allows healthcare providers to monitor patients outside of the traditional clinical setting, such as in their homes or other remote locations. This is made possible through the use of various technological devices and tools that collect and transmit patient data to healthcare professionals. RPM is especially beneficial for managing chronic conditions, keeping track of a patient's health after a hospital stay, and providing ongoing care to individuals who may have difficulty visiting a healthcare facility regularly.
Key components and features of remote patient monitoring may include:
1. Monitoring Devices: Patients typically use various medical devices, such as blood pressure monitors, glucose meters, wearable fitness trackers, pulse oximeters, and more. These devices can record vital signs, symptoms, and other health-related data.
2. Data Transmission: The data collected by these devices is transmitted securely to a healthcare provider's system. This can be done through various means, including Bluetooth, Wi-Fi, or cellular connections.
3. Data Analysis: Healthcare professionals or specialized software analyze the data received from patients to track their health status and make informed decisions about their care.
4. Alerts and Notifications: RPM systems can be set up to alert healthcare providers if a patient's vital signs or condition deviate from established thresholds, allowing for timely interventions.
5. Patient Engagement: RPM often involves patient education and engagement to help individuals better manage their own health. Patients may receive feedback, reminders, and educational resources through the RPM system.
6. Care Coordination: RPM can be integrated into a patient's overall care plan, enabling healthcare teams to collaborate and adjust treatment strategies as needed.
7. Chronic Disease Management: RPM is particularly useful for managing chronic diseases like diabetes, hypertension, heart disease, and chronic obstructive pulmonary disease (COPD). It enables healthcare providers to monitor and manage these conditions more effectively.
8. Post-Hospitalization Care: RPM can be employed to monitor and support patients after hospitalization, ensuring they are recovering well and reducing the risk of readmission.
Benefits of remote patient monitoring include improved patient outcomes, reduced healthcare costs, and increased patient convenience. Patients can receive ongoing care and attention while remaining in their familiar environments, and healthcare providers can intervene promptly if issues arise. However, RPM also presents challenges related to data privacy, technology access, and the need for healthcare professionals to manage and interpret the data effectively.
General Aim
The aim of training nurses on Remote Patient Monitoring (RPM) is to equip them with the knowledge and skills necessary to effectively use technology and remote monitoring tools to support and care for patients who are not physically present in a healthcare facility or especially at a Place -of-Care away from a healthcare facility. RPM is a rapidly evolving field that leverages technology to monitor patients' health and vital signs from a distance, in their own homes.
A growing number of remote patient monitoring systems (RPMS) are becoming popular due to the emergence of highly infectious diseases such as COVID-19, the demographic shift toward the ageing population, and the rise in health complications. Furthermore, technological advances have made RPMS more widely used. In RPMS, specific groups of patients are targeted, such as those with chronic diseases, infectious diseases during isolation, and those with mobility challenges or other disabilities. In RPMS, specific groups of patients are targeted, such as those with chronic diseases, infectious diseases during isolation, and those with mobility challenges or other disabilities[3]. The systems are also used for post-surgery patients, newborns, and elderly patients. The goal of healthcare is to keep patients as comfortable as possible during their everyday lives. Patients are, therefore, able to move freely and exercise in a private environment.[4]
New models of care are being widely investigated and trialled that could extend care into the home and prevent unnecessary acute care events. In this notion, healthcare professionals including nurses are asked to operate RPM technologies where in most cases, there is minimal training and expertise. Operating wireless diagnostic equipment that transmit data over distance, or setting up communication among parties are some of the basic skills that a nurse should have in order to support remote monitoring.
Objectives
Remote patient monitoring (RPM) is a healthcare practice that uses technology to collect and transmit patient data from a distance. The primary objectives of remote patient monitoring are to:
- Improve Patient Care:
- Ensure timely and continuous monitoring of patients, especially those with chronic illnesses or conditions, to detect early warning signs and prevent complications.
- Enable proactive and personalized care by providing healthcare providers with real-time data, allowing them to adjust treatment plans as needed.
- Enhance Patient Engagement:
- Empower patients to take an active role in managing their health by providing them with access to their own health data and educational resources.
- Foster communication and collaboration between patients and healthcare providers, which can lead to better adherence to treatment plans.
- Reduce Healthcare Costs:
- Minimize the need for frequent in-person visits, which can be costly for both patients and healthcare systems.
- Decrease hospital readmissions by identifying issues early and addressing them remotely, which can result in significant cost savings.
- Increase Access to Care:
- Extend healthcare services to underserved or remote populations, allowing them to receive care without the need for frequent travel.
- Support the aging population and individuals with mobility issues by making healthcare more accessible.
- Enhance Data Collection and Analysis:
- Collect a wealth of health data, including vital signs, medication adherence, and symptom reports, to provide a comprehensive view of a patient's health.
- Utilize data analytics to identify trends, patterns, and anomalies that can guide treatment decisions and population health management.
- Improve Quality of Life:
- Enable patients to maintain a higher quality of life by managing their health conditions from the comfort of their own homes.
- Reduce the physical and emotional burden associated with frequent medical visits.
- Early Detection and Intervention:
- Identify deteriorating health conditions or deviations from baseline parameters early, allowing healthcare providers to intervene promptly and prevent complications.
- Reduce the risk of adverse events and hospitalization.
- Population Health Management:
- Enable healthcare organizations to monitor and manage the health of a large population, identify high-risk patients, and allocate resources more effectively.
- Chronic Disease Management:
- Support patients with chronic diseases by helping them manage their conditions more effectively and reduce the burden of healthcare system resources.
- Research and Continuous Improvement:
- Enable the collection of large datasets for research, quality improvement, and the development of new treatment protocols.
- Facilitate evidence-based decision-making in healthcare by providing real-world patient data.
[1] Snoswell CL, Smith AC, Thomas EE. Video and phone consultations only scratch the surface of what telehealth has to offer. The Conversation, 2020.
[2] Malasinghe LP, Ramzan N, Dahal K. Remote patient monitoring: a comprehensive study. J Ambient Intell Humaniz Comput 2019;10:57–76. 10.1007/s12652-017-0598-x
[3] B. Talbot, et al. Patient and clinician perspectives on the use of remote patient monitoring in peritoneal dialysis Can. J. Kidney Heal. Dis., 9 (2022)
[4] T. Malche, et al. Artificial intelligence of things- (AIoT-) based patient activity tracking system for remote patient monitoring J. Healthc. Eng., 2022 (2022)
Learning Outcomes
Knowledge:
· Understand the principles and importance of remote patient monitoring
· To learn how use remote patient monitoring with telehealth
· To help patients use at-home health monitors
Skills:
To develop basic skills in assisting people in need remotely over telehealth systems.
Competence:
The acquisition of the necessary knowledge for applying telemetry at the Point-of-Care and collaborating remotely.
-
4LESSON 2 Basic of Medical Informatics
Introduction
Medical informatics, also known as health informatics or healthcare informatics, is a multidisciplinary field that combines healthcare, information technology, and data science to improve the acquisition, storage, management, and use of healthcare information. It involves the application of information and communication technology to support healthcare delivery, research, and management. Medical informatics plays a critical role in enhancing patient care, clinical decision-making, public health, and healthcare system efficiency.
General Aim
The aim of training nurses in medical informatics is to equip them with the knowledge and skills necessary to effectively use and manage healthcare information technology and electronic health records (EHRs) in their clinical practice. Medical informatics, also known as health informatics, is a multidisciplinary field that focuses on the use of information technology and data to improve healthcare delivery, patient outcomes, and the overall quality of care.
Objectives
1. Efficient Data Management: Nurses learn how to input, access, and manage patient data in EHR systems, which streamlines the documentation process and reduces the risk of errors.
2. Improved Patient Care: Medical informatics training helps nurses make better-informed clinical decisions by providing access to patient histories, test results, and evidence-based guidelines.
3. Enhanced Communication: Nurses can use electronic systems to communicate with other healthcare providers and share important patient information more quickly and accurately.
4. Decision Support: Training enables nurses to utilize decision support tools and clinical decision support systems to aid in diagnosing and treating patients.
5. Quality and Safety: Proper use of medical informatics can lead to improved patient safety through error reduction, alerts for potential issues, and medication reconciliation.
6. Research and Data Analysis: Nurses can use informatics skills to participate in research projects, analyze healthcare data, and contribute to evidence-based practice.
7. Patient Engagement: Informatics training can empower nurses to engage patients in their own care by helping them access their health information and make informed decisions.
8. Compliance: Understanding health informatics ensures that nurses can adhere to regulatory requirements and maintain the security and privacy of patient data.
9. Interoperability: Training helps nurses navigate the interoperability of various health information systems and exchange data seamlessly.
10. Continuous Learning: As technology in healthcare evolves, nurses need ongoing training to stay updated and adapt to new tools and systems.
Learning Outcomes
Knowledge:
· Get an overview of Medical Informatics and the key applications
· Explore the key uses and benefits of medical informatics in telecare and telemedicine
· To help patients use online medical systsems
Skills:
To learn and work on the Soft skills that professionals need to support productivity, creativity and collaboration.
Competence:
To learn how to manage medical systems and applications.
-
5LESSON 3 Diagnostic Equipment
Introduction
Telecare and telemedicine rely on various diagnostic equipment and technologies to remotely monitor and assess a patient's health and provide medical care or support. These devices can help detect early signs of health issues or deteriorating conditions, allowing healthcare professionals to intervene proactively and prevent hospitalization or more severe complications. Diagnostic devices can continuously or periodically collect vital health data, such as blood pressure, heart rate, blood glucose levels, and oxygen saturation. This information can be transmitted in real-time to healthcare providers, allowing them to monitor patients' conditions without the need for in-person visits.
For patients with chronic conditions like diabetes, hypertension, or heart disease, diagnostic devices enable healthcare providers to adjust treatment plans, provide timely guidance, and make medication adjustments based on remote monitoring data. Diagnostic devices can facilitate teleconsultations between patients and healthcare providers. The data collected by these devices can be shared during the consultation, aiding in a more informed discussion about the patient's condition.
By providing a more continuous and comprehensive view of a patient's health, diagnostic devices can lead to better health outcomes through early intervention and personalized care.
General Aim
Diagnostic devices play a crucial role in telecare and telemedicine, especially in community care settings, by enabling healthcare professionals like nurses to remotely monitor and assess patients' health conditions. Telecare using diagnostic devices can bring healthcare to underserved or remote communities, making healthcare more accessible to those who may have limited access to traditional healthcare facilities. Nurses can efficiently manage a larger number of patients using remote monitoring and diagnostic devices, as they can focus on patients who require immediate attention while keeping an eye on others through remote data analysis.
Diagnostic devices are invaluable tools in telecare and telemedicine for community care, benefiting both healthcare providers, such as nurses, and patients. They enhance the quality of care, increase access to healthcare services, and can lead to improved patient outcomes while reducing healthcare costs and making care more convenient.
Objectives
The objective of presenting diagnostic equipment used in telecare/telemedicine to nurses is to familiarize them with the tools and technologies that are essential for providing remote healthcare services. Telecare and telemedicine involve delivering medical care and monitoring patients from a distance, often through technology, and nurses play a crucial role in this process. Here are some specific objectives of presenting diagnostic equipment to nurses:
1. Training and Education: Nurses need to be trained in using the various diagnostic equipment and technologies used in telecare/telemedicine. They should understand how to operate the equipment, interpret results, and troubleshoot any issues.
2. Quality Care Delivery: By ensuring nurses are proficient with the diagnostic equipment, healthcare providers can maintain the quality of care they deliver to remote patients. Proper use of equipment can lead to accurate assessments and timely interventions.
3. Patient Safety: Competent use of diagnostic equipment is vital for patient safety. Nurses must know how to use the equipment correctly to prevent harm or errors in patient assessment and treatment.
4. Data Collection and Transmission: Nurses should understand how to collect patient data using diagnostic tools and transmit it securely to healthcare providers. This includes knowledge of data privacy and security practices.
5. Efficiency and Effectiveness: Proper training in using diagnostic equipment can improve the efficiency and effectiveness of nursing care in telemedicine. Nurses can make better decisions and provide more targeted interventions.
6. Communication Skills: Nurses may need to guide patients in using certain diagnostic tools remotely. Educating nurses on effective communication with patients regarding equipment usage is essential.
7. Compliance and Regulations: Understanding the regulatory and compliance requirements related to telemedicine and diagnostic equipment is crucial. Nurses need to be aware of legal and ethical considerations when using these tools.
8. Troubleshooting and Maintenance: Nurses should be able to troubleshoot common issues with the equipment and perform basic maintenance tasks to ensure its functionality.
9. Collaboration: Nurses often work as part of a team in telecare/telemedicine settings. Knowing how to use diagnostic equipment allows them to collaborate effectively with other healthcare professionals.
10. Adaptation to Technological Advances: Technology in healthcare is constantly evolving. Regular training and updates on new equipment and tools help nurses adapt to the latest advancements.
Learning Outcomes
Knowledge:
· Get an overview of the Diagnostic Equipment used to support Telecare, both medical equipment and ICT
· Learn about the basic measurements collected from peripheral diagnostic equipment
Skills:
To learn the basics of the diagnostic devices and needed ICT equipment.
Competence:
To learn what equipment to support telecare services, per needs.
-
6LESSON 4 Telemedicιne and TeleCare
Introduction
Telemedicine: Telemedicine utilizes information and telecommunications technology to transfer medical information for diagnosis, therapy and education. The medical information may include images, live video and audio, video and sound files, patient medical records, and output data from medical devices. The transfer may involve interactive video and audio communication between patients and medical professionals, or between those professionals without patient participation. Alternatively, it may simply describe the transmission of patient data either from monitoring devices (telemetry) or from medical histories (electronic patient records). Those taking part in the transfer may be located in a GP surgery, a hospital clinic or some other environment if the occasion is an emergency[1].
Telehealth: Telehealth is the use of information and communication technologies to transfer healthcare information for the delivery of clinical, administrative and educational services. Extension to include administrative healthcare information recognizes the use of telematic services to transfer demographic and operational information that may have little or no clinical content. Similarly, while distance learning courses for healthcare professionals are covered by the banner of telehealth, components of these courses may concentrate on health policy or other non-clinical topics. In contrast, the term telecare is often used to describe the application of telemedicine to deliver medical services to patients in their own homes or supervised institutions. Telecare: Telecare utilizes information and communication technologies to transfer medical information for the diagnosis and therapy of patients in their place of domicile.
Telecare allows nurses to remotely monitor patients' vital signs, chronic conditions, and overall health. This helps nurses identify potential issues early, make timely interventions, and reduce the need for frequent in-person visits.
General Aim
Nurses and care providers can provide timely care and support to patients in the community through telemedicine. They can offer advice, answer questions, and address concerns, helping patients manage their health conditions effectively. Telemedicine minimizes the need for nurses to travel to patients' homes, especially in remote or underserved areas. This can save valuable time, reduce transportation costs, and allow nurses to serve a larger number of patients. Telecare and telemedicine can bridge the gap in healthcare access for patients in rural or isolated areas. Nurses can connect with patients regardless of their location, ensuring they receive necessary care and information.
For patients with chronic conditions, telemedicine enables nurses to regularly check in, provide education, and adjust treatment plans as needed. This can help improve patients' adherence to treatment and overall health outcomes. Nurses can remotely review patients' medication regimens, offer reminders, and assess compliance. Telecare also allows for video consultations, during which patients can show their medication and ask questions, reducing the risk of errors.
Telemedicine enables nurses to consult with specialists and other healthcare professionals to provide comprehensive care to patients in the community. This collaborative approach can lead to more informed decision-making.
Objectives
Nurses play a crucial role in the use of telecare and telemedicine to provide healthcare services. The objectives of nurses using telecare and telemedicine can vary depending on the specific healthcare setting and the patient population they serve, but some common objectives include:
1. Improved Patient Access: Telecare and telemedicine help expand access to healthcare services, especially in underserved or remote areas. Nurses use these technologies to ensure that patients can receive medical advice and support without the need for physical visits to a healthcare facility.
2. Remote Monitoring: Nurses can use telecare to remotely monitor patients' vital signs, chronic conditions, and medication adherence. This allows for early detection of health issues and timely interventions, reducing hospital readmissions and improving patient outcomes.
3. Patient Education: Nurses can use telemedicine to provide patients with information and education about their conditions, treatment plans, and lifestyle modifications. This empowers patients to take an active role in managing their health.
4. Chronic Disease Management: Telecare and telemedicine enable nurses to manage chronic diseases more effectively. They can regularly check in with patients, adjust medications, and provide ongoing support to help patients manage their conditions.
5. Medication Management: Nurses can use telemedicine to help patients manage their medications, including providing reminders and addressing any concerns or side effects. This can improve medication adherence and overall treatment effectiveness.
6. Emergency Response: In cases of emergencies, nurses can use telemedicine to provide immediate guidance to patients and caregivers, helping them assess the situation and determine the appropriate course of action until in-person medical assistance is available.
7. Consultation and Collaboration: Nurses can consult with other healthcare professionals, including physicians, specialists, and pharmacists, through telecare. This facilitates collaborative decision-making and ensures that patients receive comprehensive care.
8. Reduced Healthcare Costs: Telecare and telemedicine can lead to cost savings for both healthcare facilities and patients. Nurses play a role in optimizing the use of these technologies to make healthcare more efficient and cost-effective.
9. Improved Patient Satisfaction: Patients often appreciate the convenience and accessibility of telecare and telemedicine services. Nurses can use these technologies to enhance patient satisfaction by providing timely, personalized care.
10. Preventive Care: Telecare can be used for preventive care, such as scheduling routine check-ups and screenings, and providing early interventions for potential health issues.
These objectives ultimately contribute to more efficient and effective healthcare delivery.
Learning Outcomes
Knowledge:
· Get an overview of telemedicine and telehealth in General
· Explore the benefits and limitations of telemedicine
· To learn about telemedecine data
Skills:
To learn how to handle different data formats depending the needs. To learn how to securely employ telemedecine / telehealth services.
Competence:
To learn how to securely employ telemedecine / telehealth services.







